Researchers of a study examined the gender-specific COVID-19 case fatality risks among patients with a malignant neoplasm during hospital admissions as there is little data available for gender-specific COVID-19 mortality.
Researchers of a study examined the gender-specific COVID-19 case fatality risks among patients with a malignant neoplasm during hospital admissions as there is little data available for gender-specific COVID-19 mortality.

Accessible through the CareFirst WellBeing app, these behavioral health services are working to combat health risks related to obesity.

The Office of Civil Rights published a proposed rule that could have healthcare organizations evaluating their practices surrounding, and interactions with, reproductive healthcare information.

Reasons behind asthma care lacking for low-income patients run wide. However, cost seems to be the main issue.

Bill Snyder, CEO of Vivante Health, explains how the organization's digestive health service through digital health is benefiting patients by personalizing their care and being supported in their care journey with the help of their primary care physician or gastroenterologist.

CEO of Vivante Health, Bill Snyder, shares how an integrated or "full-stack" digital health system can benefit patient care all around, amid safety concerns about digital health and the security of sensitive health information. Snyder also introduces Vivante's digestive health platform and how it's associated with the organization's digital health innovations. For example, they've invested in looking at disparate data sets and using AI and machine learning to leverage pattern recognition and recognize specific patient needs.

Over 7,000 people attended the meeting in Las Vegas this week.
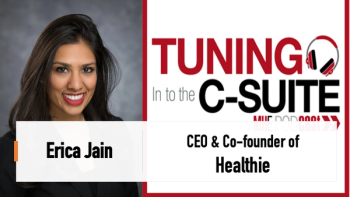
This month's episode of Tuning In to the C-Suite features Erica Jain, CEO & co-founder of digital health company, Healthie. In this discussion, Jain shared some of the challenges or things to avoid when creating a digital health startup, based on her journey with starting Healthie in 2016. She also addressed some best practices and tools that can help those working toward a digital health startup.

HealthWell to also provide best practices programming to foundation donors and patient stakeholders.

Neal Dave, executive director of Pharmacy at Texas Oncology, explained that medically related pharmacies are truly an integrated team.

In June, the Advisory Committee on Immunization Practices (ACIP) will make recommendations on the appropriate use of the vaccine in the U.S.

Pandemic-triggered changes in the healthcare industry have required hospitals, clinics, and other healthcare facilities to scale up their technology operations, resulting in high demand for tech experts.

Ed Paiewonsky, Director, Medical Outcomes Science Liaison at Alnylam Pharmaceuticals, discussed results of the Alnylam Rare Disease Trend report at this year's Asembia Specialty Pharmacy Summit.

Elizabeth Johnson, CEO of MedicoCX shared the importance of trust in healthcare and how it's been missing in drug development, marketing and delivery. Johnson said one way drug companies could build trust is including patients sooner so they're part of the process beyond clinical trials.

Kelsey Lang, principal of Avalere, breaks down the three provisions of the Inflation Reduction Act, which was discussed today at the annual Asembia Specialty Pharmacy Summit in Las Vegas.

Connie Sullivan, president and CEO of the National Home Infusion Association, addressed the benefits of home-based infusion care, the types of treatments offered to patients and its reimbursement considerations. Sullivan presented on this form of care during the Asembia 2023 Specialty Pharmacy Summit in Vegas this week.
Cate Lockhart, executive director of the Biologics and Biosimilars Collective Intelligence Consortium, shared results yesterday of a survey that look at biosimilars on the pharmacy benefit side of coverage versus medical benefit. The survey also shared how payers and those on the pharmaceutical side are anticipating the introduction of Adalimumab (Humira®), as well as what to look for in the future of the biosimilar pipeline.

But payers may be putting undue emphasis on interchangeability, said a panelist at session on biosimilars at the 2023 Asembia Specialty Pharmacy Summit.

Adam Fein, Ph.D., talked about some surprising trends in specialty pharmacy and healthcare at the 2023 Asembia Specialty Pharmacy Summit. The number of specialty pharmacy locations may be peaking. And that "gross-to-net bubble" in drug prices that Fein has written about so much — well, it may be shrinking.

Today at the annual Asembia Specialty Summit in Las Vegas, Sarah Marche, VP of Pharmacy at Highmark Health, spoke alongside other professionals from various stakeholders within the industry who are invested some way in digital therapeutics.

Cystic fibrosis drug Trikafta gets expanded indication for children ages 2-5.
Today at Asembia 2023 Specialty Pharmacy Summit in Las Vegas, Alexander Pham, VP of Client Services & Strategy at Clearway Health, talked about their collaboration with safety net hospital, OU Health, alongside the Chief Administrative Officer of OU Health, Jigar Thakkar. In this interview, Pham talked about how the Clearway and OU Health partnership helped build a specialty pharmacy program, alleviate financial burden, and more.
Ray Tancredi talked about the upcoming pipeline and more in this interview with Managed Healthcare Executive.

“It was like, we’re going to take off your head, we are going to come after you,” said Seema Verma, the Centers for Medicare and Medicaid Administrator in the Trump administration, during an on-stage interview at the 2023 Asembia Specialty Pharmacy Summit.

Despite having a highly differentiated clinical value proposition compared to branded, twice-nightly oxybates, Avadel is pricing Lumryz at $64.67 per gram or around $177,034 annually, which is on par with twice-nightly oxybate products that require chronic, middle-of-the-night awakening.

A relatively small number of cell and gene therapies have become a clinical reality. But now the specialty pharmacy industry, and healthcare more generally, is bracing for a wave of cell and gene therapies that will force change and adaption. And, yes, the new therapies will be extremely costly.

Daybue (trofinetide) is the first treatment for Rett syndrome. The pivotal trial for treatment for a lifelong condition was only 12 weeks long.

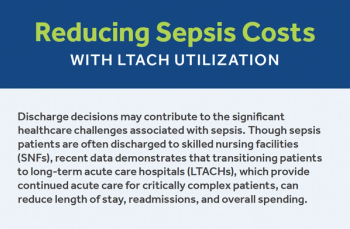
Under the fee-for-service model, it makes sense for providers and payers to withhold information. But the shift to value-based care requires the timely integration of clinical and claims information.
More than two-thirds (68%) of the respondents to the survey expressed confidence that the COVID-19 is "behind us." An overwhelming majority (80%), though, indicated that annual COVID-19 vaccination will be needed for the foreseeable future.