
ICER’s first scorecard of the barriers to fair access to medications found that more transparency is needed to fully assess insurers and their coverage policies.

ICER’s first scorecard of the barriers to fair access to medications found that more transparency is needed to fully assess insurers and their coverage policies.

Findings show substantial variation in payer-negotiated prices and self-pay cash prices at top-performing U.S. hospitals and considerable markups on clinician-administered drugs.
Across all payers, the use of generic statins has resulted in a savings of $11.9 billion annually.

Patients who are part of the Walgreen’s Prescription Savings Club can receive Semglee at up to 80% off the cash price.

OptumRx will favor the reference product Lantus on the Premium Formulary. The organization also released coverage information about other newly approved therapies.

Besremi was approved recently to treat a rare blood disease.

ICER’s review indicates that Humira’s price increases are not supported by new clinical evidence.

A reimbursement policy similar to that used for branded and generic drugs would have saved $1.6 billion from 2015 to 2019.

Smaller PBMs are rated higher by health plans in terms of satisfaction because of their ability to offer more customized solutions.

Half of the step therapy protocols for specialty drugs evaluated by investigators go beyond what is suggested in treatment guidelines.

CVS Caremark has removed 10 branded products from its formulary and added about 30 additional products.

This Tufts study has found that plans that restrict orphan drugs do so by narrowing the patient population who can receive them.

Prime’s formularies will include the insulin biosimilar over the reference product Lantus beginning in January 2022.

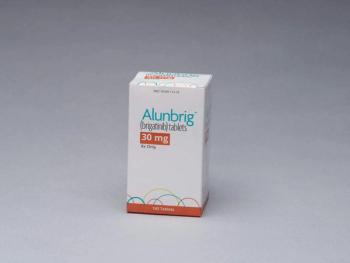
Several generics of the cancer therapeutic are available.

EmsanaRx, the new PBM, aims to provide large employers with flexibility and transparency on drug spending.

Specialty drug prices are rising as these therapeutics replace lower-cost therapies.

Cigna plans to remove 45 drugs from its Standard Prescription Drug List and add restrictions for other therapeutics.

Cumulative spending on drugs without overall survival data was $1.8 billion in 2018 and surpassed that of drugs with such data.

Specialty medicines are now 53% of spending, up from 27% in 2010 and driven by growth in autoimmune and oncology therapies.
If a patient does not remain on the drug for at least three months due to effectiveness or tolerability, a significant portion of the drug cost will be refunded to Point32Health.

Treating and managing patients with paroxysmal nocturnal hemoglobinuria is expensive and requires constant surveillance by the provider and health plan.

AmerisourceBergen/Xcenda survey finds payers believe biosimilars provide costs savings, and they are expected to continuing contracting with manufacturers.

Express Scripts will put the first interchangeable biosimilar insulin on its National Preferred Formulary and exclude Lantus, the reference product.

Most of the solutions have established systems to track patient outcomes over time, and several include performance guarantees as part of their solution.

This is the second specialty pharmacy selected to distribute Tavneos, a first-in-class, oral therapy to treat a group of autoimmune diseases characterized by inflammation and damage to small blood vessels.