Pharmacy
Latest News
Latest Videos

Podcasts
CME Content
More News

The deliberate disconnection of Change Healthcare to ring fence a cyberattack entered its seventh day today. Prescribers are finding ways to get pharmacy claims processed, and UnitedHealth Group says disruption to the dispensing of prescriptions has been minimal. But independent pharmacies want more information and protection from financial consequences from pharmacy benefit managers.

The information systems of Change Healthcare, a recently acquired subsidiary of UnitedHealth Group, were disconnected on Wednesday.

Healthcare beyond the doors of the doctor’s office has the potential to offer more care to more people. But payers need to think about how to ensure that care is consistent. Regardless of the setting, care decisions must be based on evidence-based content and supported with strong patient education.

Dario is using Sanofi’s research infrastructure to evaluate its digital health products.

Tony Little, ND, VP of Solutions Architecture at Prescryptive Health, shares how the organization is tackling one of the biggest barriers to prescription adherence — cost — through a digital app, among the other barriers patients face.

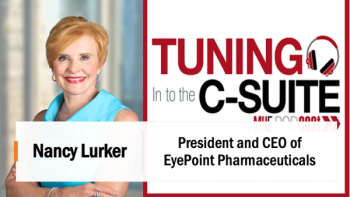
The Magellan Rx Management CEO is replacing Ken Paulus, who held the top job at Prime since May 2019.

7 of them launched during the first several days of July, joining Amgen's Amjevita in the suddenly crowded market of Humira competitors. Pfizer’s Abrilada is the only FDA-approved Humira biosimilar that hasn’t launched.

The Sandoz's and Boehinger Ingelheim's Humira biosimilars will join Amgen's Amjevita on the formulary of UnitedHealth Group's PBM. Cyltezo may have a marketing edge because of its interchangeability designation.

Vanderbilt’s Stacie Dusetzina and colleagues explain how the ‘copay adjustment’ programs work in this week’s JAMA Internal Medicine and also shed light on third strategy used by insurers and pharmaceutical benefit managers, the alternative payment program.

Neal Dave, executive director of Pharmacy at Texas Oncology, explained that medically related pharmacies are truly an integrated team.

Kelsey Lang, principal of Avalere, breaks down the three provisions of the Inflation Reduction Act, which was discussed today at the annual Asembia Specialty Pharmacy Summit in Las Vegas.
Cate Lockhart, executive director of the Biologics and Biosimilars Collective Intelligence Consortium, shared results yesterday of a survey that look at biosimilars on the pharmacy benefit side of coverage versus medical benefit. The survey also shared how payers and those on the pharmaceutical side are anticipating the introduction of Adalimumab (Humira®), as well as what to look for in the future of the biosimilar pipeline.

Daybue (trofinetide) is the first treatment for Rett syndrome. The pivotal trial for treatment for a lifelong condition was only 12 weeks long.

Aside most of the 311 respondents to the 2023 Annual Managed Healthcare Executive Pharmacy Survey favoring PBMs, two-thirds indicated they favor restrictions on rebates and discounts so PBMs won’t favor drugs with high discounts. A similar proportion favor transparency rules that would require disclosure of rebates and discounts.

Results show that beliefs about biosimilars are mixed

Vast majority of respondents indicate that CMS price negotiation is a positive development

COVID-19 is viewed as the condition putting the most upward pressure on drug expenditures, but over the next five years, respondents are eyeing migraine and hematologic cancers.

The Senate Finance Committee released a framework for legislation this week, and the leaders of the “big three” PBMs are scheduled to be witnesses at another committee's hearing about insulin prices on May 10.
A Senate Finance Committee hearing yesterday was the latest in a series of hearings and announcements featuring sharp condemnation of the business practices of the large pharmacy benefit managers.

Managing Directors of L.E.K. Consulting, Joe Johnson, Todd Clark and Brendan Mitchell introduce the innovations happening in pharmacy, more specifically disruptive innovations, and how they affect managed care. The team explained some of the innovations to be on the lookout for in the future, also.

The Academy of Managed Care Pharmacy is throwing its support behind federal legislation that would create a Medicare benefit category for prescription digital therapeutics.

Specialty drugs are expected to comprise 80% of the FDA approvals this year. Among them are gene therapies for hemophilia A and Duchenne muscular dystrophy priced at between $2 million and $3 million.

Coverage decisions about prescription digital therapeutics may take payers out of their comfort zones and require new processes and subject matter experts, according to members of a panel at the AMCP annual meeting. But P&T committees are likely to still be central to the process.

They are the trendy way to lose weight and payers have been noticing an increase in GLP-1 claims. An analysis of the pharmacy and healthcare claims of a small commercial health plan in Texas documents the growth in the off-label usage of the GLP-1s, such as Ozempic, for weight loss.

The IQVIA vice president sees trouble for generics manufacturers, but painted a bright picture for biosimilars during his keynote address at the annual meeting of the Academy of Managed Care Pharmacy (AMCP).