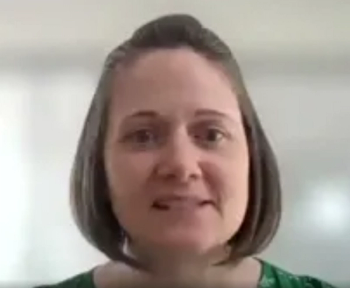
Melissa A. Soliz, J.D., of Coppersmith Brockelman PLC is one of 12 winners in this year's Emerging Leaders in Healthcare feature. In an interview with MHE, Soliz recommends the book, “The Immortal Life of Henrietta Lacks” by Rebecca Skloot to those in healthcare because "it is a compelling portrayal of how the law, ethics, ownership and business interests, and health inequities impact patient care and the advancement of that care from a generational perspective."