
Some study results tempered enthusiasm for one digital therapeutic but others are showing promising if early results.

Some study results tempered enthusiasm for one digital therapeutic but others are showing promising if early results.

Less than a quarter of menopausal women have their menopause symptoms entered into their charts at primary care visits, resulting in missed opportunities for timely treatment.

Treatment with Entyvio (vedolizumab), an integrin receptor antagonist, followed by Humira (adalimumab), a tumor necrosis factor blocker, resulted in the lowest overall incidence of adverse events, according to an industry-sponsored study.
Sen. J.D. Vance credited Donald Trump with "salvaging" the Affordable Care Act (ACA). Gov. Tim Walz said Trump worked to repeal the ACA and Vance has proposals that would bring back pre-ACA limitations on health insurance for people with preexisting conditions.

With this year's Breast Cancer Awareness Month now underway, we are sharing eight facts and updates about breast cancer that you might not know about.

In 2025, Aetna will merge its three stand-alone prescription drug plans into a single plan and member cost-shares will be consistent at every pharmacy within its network.

Otulfi is the fourth Stelara biosimilar to be approved by the FDA.
Most people haven’t heard of the condition, but Friedreich’s ataxia is getting more attention because of a new treatment and a large number of clinical trials enrolling people with the condition.

Here’s what you missed this week on Managed Healthcare Executive.
The Democrats have expanded the program under the Affordable Care Act. Republicans have proposed cuts in federal funding and work requirements.
Neither party wants to be perceived as threatening the overall Medicare program. The Biden administration did take steps to reduce payment to Medicare Advantage plans. Insurance companies objected, but some industry observers said it was an overdue correction.

Employment satisfaction, sleep quality and lack of physical movement were all tied to vitality levels, survey results show.
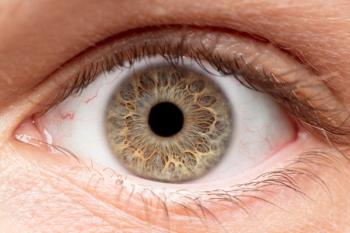
The Phase I/II trials for rare forms of hereditary blindness further confirmed the potential for gene therapy treatments of congenital diseases of the retina.

The patient panels of physicians underrepresented in medicine (URiM) showed that they had greater odds of being a Medicaid provider than White family physicians.
Aqneursa is the second drug approved within a week to treat Niemann-Pick Disease, Type C.

A study found omitting a course of antibiotic prophylaxis was non-inferior to the routinely administering antibiotics in patients undergoing allogeneic hematopoietic stem cell transplantation.

Novo Nordisk said it’s open to discussions with PBMs based on their commitments that a lower semgalutide list price would not impact formulary coverage.

The FDA has already approved Zoryve cream (0.3% and 0.15%) for plaque psoriasis and atopic dermatitis in adults and children ages 6 and up. Currently, Zoryve foam 0.3% is only approved to treat seborrheic dermatitis in adult and pediatric patients 9 years and older.

This is the first FDA approved medication for the rare and progressive neurodegenerative disease, Niemann-Pick Disease Type C.
Bimzelx was first approved last year for the treatment of moderate to severe psoriasis in adults, making it the first and only IL-17A and IL-17F inhibitor approved in the United States for four autoimmune diseases.

New anecdotal evidence suggests some chemoimmunotherapy treatments may improve pulmonary arterial hypertension symptoms, but the overall evidence remains murky.

Results looking at the first season of RSV use shows that it is 75% effective at preventing RSV-associated hospitalizations in those 60 and older.

Studies conducted in Taiwan and the United Kingdom have added to. the evidence that inherited genes play a prominent role in the development of treatment-resistant depression.

Here’s what you missed this week on Managed Healthcare Executive.

Today’s approval means that FluMist is the first pharmacy-prescribed influenza vaccine that does not need to be given by a healthcare professional.

Participants cite the recent, ongoing popularity of GLP-1 drugs prescribed for weight loss.

A news release about the complaint says the "big 3 " pharmacy benefit managers — CVS Caremark, Optum Rx and Express Scripts — have kept hundreds of millions of dollars of rebates while excluding insulin products with lower list prices from their formularies.

“Cure” is not an immutable term, the authors of a new study write, and its meaning depends on the context in which it is used. Sometimes, it shouldn’t be.

Study of 29 children treated with Zolgensma (onasemnogene abeparvovec) shows mixed results.

Three different doses of Niktimvo all had high rates of response among patients with recurrent or refractory graft-versus-host disease (GVHD).