Business Strategy
Latest News

Latest Videos
Podcasts
CME Content
More News

How Healthcare Leaders Can Have the Greatest, Most Sustainable Impact on Vulnerable Populations
Congress’ Medicare and public health emergency extensions prove to be beneficial for vulnerable communities, and leaders have the opportunity to create a lasting impact.



Sharing technologies like blockchain could help healthcare institutions establish a consistent, accurate, and trustworthy approach to data collection and dissemination.

The case concerns the controversial direct and indirect remuneration (DIR) fees that pharmacy benefit managers (PBMs) collect from pharmacies. Meanwhile, a separate whistleblower lawsuit has been filed against CVS Caremark, its parent company and SilverScripts, its Part D plan, accusing them of blocking customers from getting cheaper generic drugs.

Health systems with more primary care doctors and palliative care services saw fewer people coming back to the hospital, a new study finds.


As many asme 14 million people with Medicaid coverage stand to lose their health insurance when the COVID-19 public health emergency ends.

Legislation that would establish benefit categories for digital therapeutics has been introduced in Congress.

To thrive organizations must figure out how to build and maintain a strong culture in an increasingly remote workplace, and implement effective recruitment and retention strategies in an economy where there are fewer workers.

If biosimilar acceptance is to grow, it’s going to take a great deal of work to improve the levels of trust between payers, patients, and oncologists.

The review, partly funded by Amgen, the maker of Riabni, makes the case for using the biosimilar to Rituxan for all indications of the originator.

The guide is designed to help spread best practices and help healthcare decision-makers understand the benefits of digital therapeutics.

Pharmacy benefit managers can help health plans understand when to best leverage and align to biosimilars and other cost-effective treatments, argues Prime Therapeutics' Kelly McGrail-Pokuta.

A recent HHS Office of Inspector General's report found that Medicare Advantage (MA) plans inappropriately deny prior authorization requests. With MA enrollment growing, scrutiny of MA plans and their utilization management strategies is also likely to grow, according to Alina Czekai, M.P.H., of Cohere Health. Czekai argues that artificial intelligence and machine learning can improve utilization management and prevent inappropriate denials.

In their general session, Adam J. Fein, PhD of Drug Channels Institute, and Doug Long of IQVIA reviewed the current specialty pharmacy space, ongoing trends and future expectations.
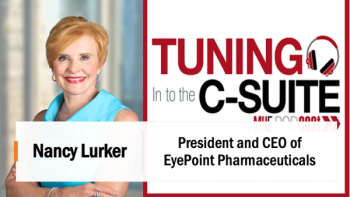
Briana Contreras, editor of Managed Healthcare Executive, spoke with Nancy Lurker, CEO and president of EyePoint Pharmaceuticals. Nancy shared a bit about EyePoint and how the organization’s innovative therapies are addressing patient needs through eye care, and most importantly, she addressed C-Suite positions like the CEO role. Nancy shared advice for those seeking to reach the CEO level, especially toward women in healthcare and other roles, and what it takes to run a biopharma company.

Accurate data and comprehensive analysis enable health plans and healthcare providers to advance the safe use of medication.

Significant changes to Star Ratings are in store for 2023, which will directly impact health plans in many ways. For example, their ability to market to members year-round. Included are three things health plans should act on now to maintain or boost quality scores, plan growth and retention, and financial health.

Patient deductibles are likely to continue rising in coming years, and healthcare providers will have to implement strategies to continue providing patients with the best possible care.

As of early this year, as many as 23 million Americans may have developed long COVID, in which symptoms persist four or more weeks after first being infected with the virus. The condition is likely to have additional long-term effects that are not yet clear. However, the U.S. has begun to obtain a glimpse of long COVID’s far-reaching impact on those who suffer from it - and the picture is rather disturbing.

As personalized medicine grows, so does the need for specialized management of laboratory testing.

Patients are likely to continue to choose to recover at home rather than go to skilled nursing facilities, according to a new report by Trella Health.

There is no lack of available COB solutions on the market, and the trouble is often identifying which option is the best fit for your organization. For optimal results, look for the following six elements in a COB solution to have the most success.

Equity is a central part of healthcare quality, but health plans often lack information on individual members’ race and ethnicity, making assessing and improving health outcomes challenging.