
Immediately after the FDA said it found elevated levels of the carcinogenic ingredient N-nitrosodimethylamine (NDMA) in certain extended release (ER) metformin products, the first 2 major recalls are underway.

Immediately after the FDA said it found elevated levels of the carcinogenic ingredient N-nitrosodimethylamine (NDMA) in certain extended release (ER) metformin products, the first 2 major recalls are underway.

Jeffrey Skolnik, MD, vice president, clinical development of Inovio Pharmaceuticals Inc Discusses Glioblastoma Treatment in ASCO interview.

Adrian Kilcoyne MD MBA MPH, vice president, US Medical Affairs and HEOR, oncology, AstraZeneca, discusses a paradigm shift in lung cancer treatment due to the overwhelming efficacy of the EGFR-TKI treatment.

A digital-first strategy is a way to navigate through the COVID-19 storm.


Despite heroic efforts by hospitals across the country, the healthcare supply chain has struggled in the fight against COVID-19.

Tagrisso, the targeted therapy made by AstraZeneca, could become the treatment of choice for the majority of lung cancer patients with mutations in a certain gene who are treated after surgery, based on findings presented this past weekend at the American Society of Clinical Oncology annual meeting.

Keytruda, the immunotherapy with more than 20 indications in both blood and solid tumor cancers, doubled rates of progression-free survival for certain patients with metastatic colorectal cancer, according to results presented Sunday at the American Society of Clinical Oncology annual meeting.


During the American Society of Clinical Oncology 2020 Annual Meeting, Flatiron Health, Foundation Medicine, and Genentech will be presenting plans for the Prospective Clinico-Genomic study (PCG), a low-interventional pilot that will use a technology-enabled prospective data collection platform to simplify data collection for patients with lung cancer being treated through clinical trials. The idea is collect blood samples using Foundation Medicine’s liquid biopsy assay and analyze the results through Flatiron’s platform, to see if genomic changes can be detected over the course of cancer treatment. Bobby Green, MD, chief medical officer for Flatiron Health, spoke with Managed Healthcare Executive®.

Managed Healthcare Executive recently had a wide-ranging conversation with de Brantes about COVID-19, the healthcare sector and how the precipitous drops in utilization and provider revenue may affect the future of bundled payment and other alternative payment models.
Anna Lee, lead author of the abstract: Changes in Cancer Mortality Rates After the Adoption of the Affordable Care Act, discusses her study with MHE. Lee presented her study May 29 during ASCO 2020's virtual conference.

Sara Douglas, lead investigator of the Abstract: Video Conference Intervention for Distance Caregivers (DCGs) of Patients with Cancer: Improving Psychological Outcomes, discusses her study with MHE's Briana Contreras which will be presented at ASCO 2020.
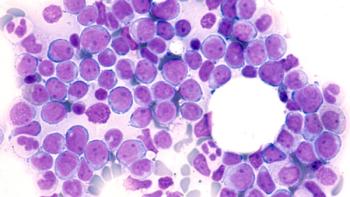
A fresh look at MURANO data, released this week at the American Society of Clinical Oncology 2020 Annual meeting, shows the poor outcomes that result when patients halt treatment for good, and highlight the need to manage doses carefully to avoid toxicity.

The 2020 annual meeting of the American Society of Clinical Oncology that launches today will feature the first results from CITYSCAPE, a trial involving a novel immunotherapy approach in non-small cell lung cancer (NSCLC). This phase 2 trial is the first to combine the immunotherapy tiragolumab with atelzolizumab (Tecentriq), the monoclonal antibody that targets the programmed cell death ligand-1 (PD-L1).

IV artesunate is the only drug available in the U.S. to treat the disease.

Healthcare providers have increasingly entered into value-based contracts with payers in recent years because they offer the opportunity to increase revenue-the primary driver of change for any business.

Cardinal Health Oncology survey shows oncologists want more training to care for growing number of cancer survivors.

Managed Healthcare Executive recently had a wide-ranging conversation with de Brantes about COVID-19, the healthcare sector and how the precipitious drops in utilization and provider revenue may affect the future of bundled payment and other alternative payment models.

Minnesota health insurance executive shares his belief that healthcare utilization peaks and valleys because of COVID-19, with MHE Senior Editor Peter Wehrwein.

As the world has gone virtual during the coronavirus pandemic, so has healthcare. Digital transformation has accelerated at warp speed, with virtual care delivery going from rare exception to operating norm almost overnight.

The novel coronavirus crisis has abruptly upended the operations and behaviors of both businesses and consumers-with such changes seemingly just the beginning.

Concerned about neglected healthcare and spike in deaths, physicians’ public service nationwide campaign urges senior patients, “don’t neglect your health” in a video.

Dr. Charity provides mental health support and advice to the growing number of burned out health workers.

Despite facing challenges such as limited access to personal protective equipment (PPE) following the COVID-19 outbreak, radiation oncology clinics quickly implemented safety and process enhancements that allowed them to continue caring for cancer patients.


Physician Performance LLC’s Weekly Zoom Clinical Call fills physicians in about the initial steps of palliative care.

Doctor.com announced the launch of VirtualVisit - a new telemedicine solution that enables any provider to start practicing medicine virtually in less than 5 minutes, completely free of charge.

It’s difficult for people seeking mental health treatment to get it right now. COVID-19 has effectively halted most non-essential doctors’ visits and accessing behavioral health treatment is even more challenging than in the past due to limitations with residential treatment and outpatient group sessions.