Fitusiran May Open Doors for Treatment of Multiple Women’s Bleeding Disorders
University of Pittsburgh’s Margaret Ragni, M.D., M.P.H., discussed fitusiran, the investigational small interfering RNA (siRNA) therapeutic, with Managed Healthcare Executive and also some of the possible limitations of gene therapy for hemophilia.
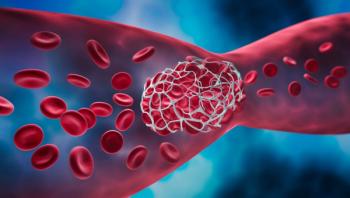
The therapeutic value of fitusiran, an investigational small interfering RNA (siRNA) therapeutic for hemophilia A and B, is its ability to make more thrombin available for clotting, and this opens doors not only in hemophilia care but also in women's bleeding disorders that for one reason or another are often overlooked,
Ragni is director of the Hemophilia Center of Western Pennsylvania and professor of medicine and translational research in the Division of Hematology and Oncology at the University of Pittsburgh.
In recently published phase 3 studies, Fitusiran was able to significantly reduce bleeding in hemophilia A and B (89.9%-90.8%), even in patients with inhibitors to clotting factor VIII or IX (FVIII, FIX). The drug “silences” antithrombin to allow background thrombin to produce clots more readily.
Related:
“A long time ago, it was recognized that people with antithrombin deficiency had much less bleeding tendency. In fact, they had clots,” Ragni explained. “So, one of the thoughts was how do we harness that regulatory capability of the antithrombin to allow patients to have less bleeding?”
siRNA molecules are parts of RNA that block or “silence” the expression of certain genes. Fitusiran works by silencing the gene responsible for antithrombin, which plays a crucial role in blood clotting.
For patients who depend on FVIII and FIX replacement therapy administered several times a week, fitusiran demonstrated potential as a once-monthly prophylactic treatment able to control bleeding without peaks or troughs in active drug levels. Even fewer injections may be viable, Ragni said.
“Actually, it's now being looked at as every other month to provide a safety net against thrombosis,” she said. “It's been shown that if you can maintain that antithrombin level no lower than 20%, you can avoid thrombosis, so it's an incredible option to take a subcutaneous drug once every 2 months, perhaps maybe 6 times a year, and avoid bleeds, whether you have an inhibitor or not.”
Although hemophilia is generally thought of as a male disease, women have symptoms, too, often associated with mild or moderate hemophilia, owing to below-normal levels of FVIII and FIX. Heavy menstrual bleeding may be hemophilia-related and go undiagnosed. The same is true in
Emerging agents such as fitusiran offer hope for better care for the female gender with these conditions, Ragni said. “We really want to assure that women who have bleeding disorders and are at risk for perhaps more bleeding than men because of their gynecologic situation — heavy menstrual bleeding, postpartum bleeding — have access to these novel therapies.”
For women on hormone therapy who are prescribed clotting agents, there is potential for complications, which means that investigators do need to look at women separately from men in studying the utility of these novel agents, Ragni said. She called for more clinical trials enrolling women, with an eye to safety.
“First and foremost is safety in women and a lack of tragic effects. And this also begs the question are these drugs safe in the setting of hormone use? If you perturb coagulation, would you be in any way potentially causing side effects?” Ragni asked.
Although fitusiran, if approved could be a major clinical advance, in terms of reduced administrations, recently approved once-weekly Altuviiio (efanesoctocog alfa) is a half-life extender for hemophilia that has been a revolution in its own right, Ragni said: “The change from the burden of three times a week to once a week is really astounding.”
“And,” she continued, “I think there's a lot of excitement about one-and-done, which is how they talk about hemophilia gene therapy in my clinic — you know, how can we avoid IVs altogether and have a — quote —normal life and no fears of bleeding or having to stop everything and take factor?”
Gene therapy for hemophilia still requires a good deal of development work. About 80% of patients have a short-term abnormality of liver function, which can be addressed with steroids, she said. If the steroids don't work, there is a danger that gene therapy will not succeed.
Another shortcoming of gene therapy is that up to 50% of patients aren't eligible for use of the adeno-associated viral vector used to convey DNA to target cells. “You can't take gene therapy because your body would inactivate it,” she noted.
Young children also are not eligible for gene therapy, but much research is ongoing and there is potential that messenger RNA may help accomplish genetic modification without liver toxicity or age issues.
“We'll have to wait and watch, but I think we're going to be seeing some revolutionary changes in the next decade for these diseases,” Ragni said.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.