Rules for independent review mirror current state policies
Current state policies vary greatly, however, and new standards for external review could drive up costs
Key Points
PROVIDING AN EXTERNAL review process for denied claims is routine for most insurers. Current state policies vary greatly, however, and new standards for external review could drive up costs, experts say.
Under the Patient Protection and Affordable Care Act (PPACA), insurers are now mandated to provide beneficiaries the option of an external, independent review of denied claims. As part of the provision, group health plans and health insurance issuers must comply with respective state external-review processes as long as the state policy includes the minimum consumer protection standards outlined in the Uniform Health Carrier External Review Model Act.
If the state process doesn't meet the minimum standards, group plans, health insurers and plans in the individual market within the state would need to implement an effective external review that meets the minimum federal standards.
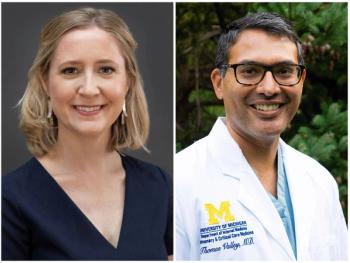
According to Katie Dunton, an assistant research professor at the Georgetown University Health Policy Institute, external reviews are typically offered by insurers voluntarily. Forty-four states also require that external reviews are provided as an option for denied claims, she says.
Even so, state policies vary. Dunton says PPACA will provide uniformity to the external review process. The regulations will also give self-funded ERISA plans an option for appeal that won't have them heading to the courtroom.
"It's not that every state has to have the same [policy], it's just the minimum level of protection that consumers should have," Dunton says.
"It is going to increase the cost," he says. "It's going to increase the inconvenience to the providers of service, and it's not going to provide the intended consequence to the patient of getting a higher rate of approved claims."
A report from the United States Government Accountability Office released in March found that when reviewing appeals data from four states, insurers reported reversing their original coverage denial in 39% to 59% of cases. The report also referenced another national study conducted by America's Health Insurance Plans that found a reversal rate of about 40% after independent, external reviews.
Further, the study also tracked application denials and found variation by age in a wide range of 5% to 29%.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.