- Drug Coverage
- Hypertrophic Cardiomyopathy (HCM)
- Vaccines: 2023 Year in Review
- Eyecare
- Urothelial Carcinoma
- Women's Health
- Hemophilia
- Heart Failure
- Vaccines
- Neonatal Care
- NSCLC
- Type II Inflammation
- Substance Use Disorder
- Gene Therapy
- Lung Cancer
- Spinal Muscular Atrophy
- HIV
- Post-Acute Care
- Liver Disease
- Pulmonary Arterial Hypertension
- Safety & Recalls
- Biologics
- Asthma
- Atrial Fibrillation
- Type I Diabetes
- RSV
- COVID-19
- Cardiovascular Diseases
- Breast Cancer
- Prescription Digital Therapeutics
- Reproductive Health
- The Improving Patient Access Podcast
- Blood Cancer
- Ulcerative Colitis
- Respiratory Conditions
- Multiple Sclerosis
- Digital Health
- Population Health
- Sleep Disorders
- Biosimilars
- Plaque Psoriasis
- Leukemia and Lymphoma
- Oncology
- Pediatrics
- Urology
- Obstetrics-Gynecology & Women's Health
- Opioids
- Solid Tumors
- Autoimmune Diseases
- Dermatology
- Diabetes
- Mental Health
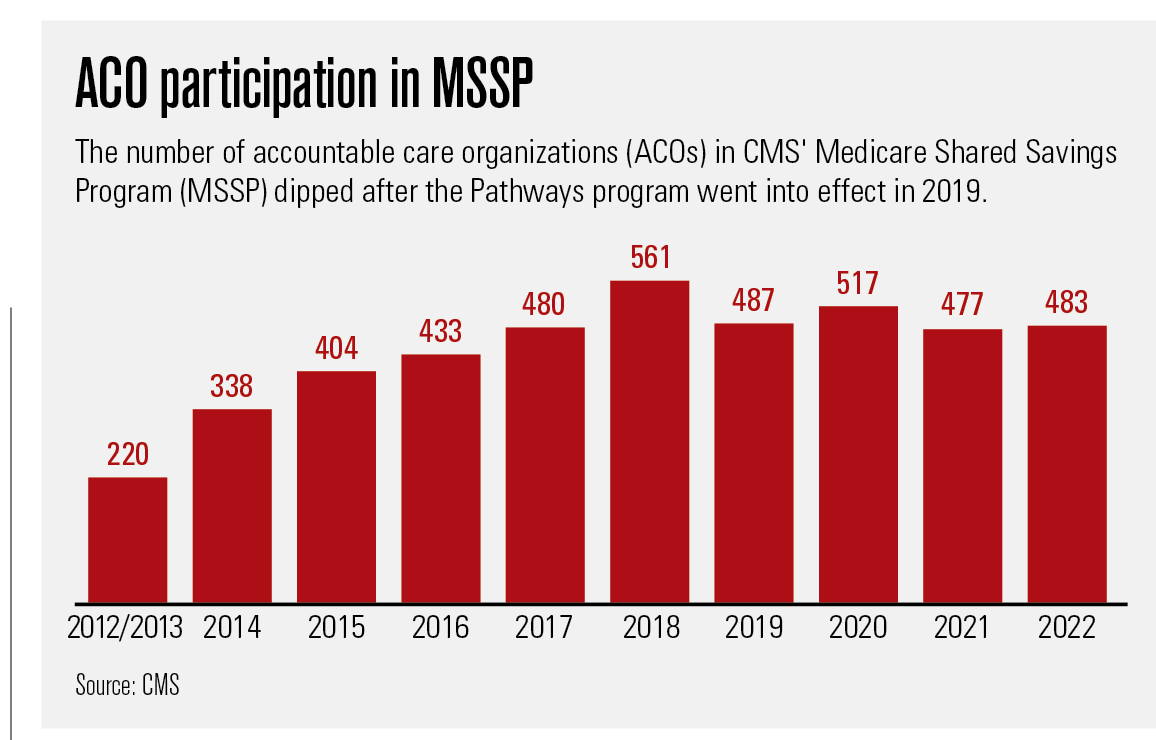
ACO Update: The Pathways to Success Program
The program implemented by the Trump administration is designed to put more Medicare Shared Savings Program ACOs into two-sided risk. An industry group has discouraged participation in the program.
Since its inception in 2012-2013, the CMS Medicare Shared Savings Program (MSSP) has cranked along like a roller coaster climbing steadily upward. Starting with 220 participating accountable care organizations (ACOs) and 3.2 million beneficiaries, it reached the high point in 2018 with 561 organizations covering 10.5 million people.
That was the same year that CMS unveiled Pathways to Success, its overhaul of MSSP’s ACO program aimed at increasing cost savings for the Medicare program by requiring more MSSP ACOs to assume two-sided risk: upside “shared savings” if they come in under budget for their attributed population but also downside “shared losses” if they go over it. The number of participating ACOs fell to 487.
Since then, the MSSP ACO program has oscillated between shallow valleys and modest peaks of ACO participation, growing by 30 organizations in 2020, losing 40 in 2021, and adding 6 this year. The number of beneficiaries covered has, though, held relatively steady with 11 million at the beginning of this year, or about one-third of the 33 million beneficiaries in traditional Medicare.
A number of factors contribute to those numbers, including the normal ebb and flow of ACOs joining and leaving the program and consolidation of providers. The winding down of another CMS ACO program, called Next Generation, had some ACOs looking for a new home.
Then there is what David Muhlestein, Ph.D., J.D., calls the “really big driver”: the COVID-19 pandemic.
“It has made people completely rethink what their priorities are, and anything related to ACOs is just so much less important right now,” says Muhlestein, chief strategy and chief research officer for Leavitt Partners, a healthcare consulting firm in Salt Lake City.
Jennifer Gasperini, director of regulatory and quality affairs for the National Association of ACOs (NAACOS) agrees that the pandemic and all those other issues are at play. But the way she sees it, Pathways is the main reason.
“We definitely think that Pathways has had an effect on the overall interest in the program,” she says. “Pathways decreased the incentive to participate by doing two things: reducing the shared savings that you can keep if you are successful and pushing (ACOs) to risk more quickly.”
Industry observers say it can take an ACO at least three years to get its sea legs. That timeline is about right, Muhlestein says. But CMS, he notes, is looking at a different timeline and issue: saving Medicare, a program under financial stress as it takes on the baby boom: “If you have a bunch of organizations that won’t take downside risk and will only stick around as long as there is a possibility of getting payment, can you say they are really making substantive changes to improve care and lower costs?”
Two-sided risk sooner rather than later
Accelerating assumption of two-sided risk is the most important difference between the Pathways program implemented by the Trump administration and the original MSSP. Pathways sorted the prior MSSP’s multitrack options down to two, Basic and Enhanced, although the Basic Track has five stages. ACOs newly entering the Basic Track have a two-year period of upside-only risk and 40% shared savings. After that, they are on a three-year schedule of two-sided risk that dials up the shared-savings percentages but also creates greater exposure to shared losses.
The Enhanced Track puts ACOs right into two-sided risk with shared savings of 75% and shared losses of between 45% to 75%. But, importantly, the Enhanced Track also qualifies the ACO as an Advanced Alternative Payment Model, which makes it eligible for incentive payments under a different CMS program.
ACOs that were participating in MSSP prior to Pathways could enter the Basic Track at its various stages depending on their revenues, how long they had been participating in MSSP and other factors. According to a CMS report earlier this year, as of Jan. 1, 2022, 337 of the 483 (70%) ACOs in the Pathways version of MSSP were participating in the program’s Basic Track, and 190 (56%) of those were still in the two-year period of one-sided risk. The other 146 jumped right into the Enhanced Track.
David Muhlestein

Muhlestein is a fan of the Pathways effort to push ACOs into assuming two-sided risk sooner: “I think that making people move toward risk makes it real and requires them to think about things in a way they probably didn’t before,” he says. “I think, basically, it says quit experimenting and start doing, which is a major difference (from) what has happened in the past.”
The Pathways rules also changed some of the benchmarking methods used to set the financial goals of the ACOs and therefore their eligibility for shared savings and losses.
Although NAACOS generally approves of CMS’s benchmarking changes, the group is concerned about what Gasperini dubs the “rural glitch.” For instance, an ACO representing half the care in a smaller region may improve by 5% in a year. That means that, on average, the whole region improved by 2.5%. By exclusively comparing the ACO to its region, the ACO is literally competing against itself.
“This is about the idea of having to constantly kind of beat yourself,” Gasperini says. “That is one issue that we think, if changed, could really go a long way toward sustainability in the program.”
Pathways rules have some benefits for the participating ACOs. They can also permit the bypass some Medicare restrictions on telehealth services. (Because of the COVID-19 Public Health Emergency and its telehealth waivers, the telehealth perk hasn’t meant as much as it might have). Additionally, Pathways waives a Medicare rule that limits coverage of rehabilitation in a skilled nursing facility to beneficiaries who were discharged to the facility after three consecutive days in a hospital. The Pathway rules also allow ACOs to make $20 incentive payments to beneficiaries to take steps such as joining a wellness program that are believed to lower costs and reduce the risk of serious illness.
NAACOS has viewed the declining number of ACOS in MSSP with alarm. When the CMS released the figures earlier this year, NAACOS issued a press release that quoted its chief executive officer, Clif Gaus, Sc.D., M.H.A., as saying they showed a “shrinking of this important ACO model.” According to NAACOS, 18 of 46 new ACOs participating in the program are former Next Generation participants and so not really new ACOs.
Many of NAACOS’ concerns would be remedied if a bipartisan bill stalled in the House were to gain traction. Introduced in July 2021, the Value in Health Care Act of 2021 would bump MSSP’s Basic Track shared-savings rate back to 50% and give ACOs at least three years in the one-sided risk mode.
Meanwhile, NAACOS continues to meet with the Biden administration to discuss adjustments to MSSP ACO, including new incentives and grants that would help attract practices. The administration, Gasperini says, is “engaged with us and, I think, committed to value-based care, and hopes it or CMS, or Congress, will make some changes to Pathways before the end of the year. Now it’s really about putting pen to paper and making some of these changes so that we can see increased participation.”
Like Gasperini and NAACOS, others are also waiting to see which direction the Biden Administration takes with the ACO program.
“The big one is what is the Biden administration plan?” says Muhlestein. “That is really going to influence in the next couple of years how much activity takes place and how active people are. I would fully expect them to come up with a full plan, both from the (CMS) Innovation Center as well as CMS for the MSSP.”

Doing More and Saving More with Primary in Home Care
September 1st 2021In this week’s episode of Tuning In to the C-Suite podcast, MHE Associate Editor Briana Contreras interviewed VillageMD’s Senior Medical Director of Village Medical at Home, Dr. Tom Cornwell. Dr. Cornwell discussed the main benefits of primary care at home, which includes the benefit of cost savings for patients, maintaining control of hospital readmissions and others. Dr. Cornwell also noted what has changed in the industry of at-home care and if there has been interest from payers like insurance companies and medicare in the service.
Listen
