6MWT oxygen recovery may improve risk stratification in fibrotic ILD
Key Takeaways
- Prolonged recovery from exertional desaturation in fILD patients indicates worse baseline lung function and higher disease progression risk.
- A novel recovery index (RI) integrates desaturation degree, recovery time, and supplemental oxygen use, offering prognostic insights.
A team of Researchers developed a "recovery index" that integrates three factors related to the six-minute walk test.
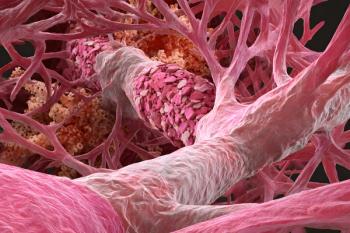
Patients with fibrotic interstitial lung disease (fILD) often face an unpredictable clinical course marked by progressive lung function decline and an elevated risk of death or lung transplantation.
Although exertional oxygen desaturation during a six-minute walk test (6MWT) has long been recognized as a marker of poor prognosis, new research from investigators at McMaster University in Hamilton, Ontario, Canada, suggests that how quickly patients recover from that desaturation may offer additional, clinically meaningful insight into disease severity and progression.
The study findings, published online Dec. 30, 2025, in Chest, revealed that prolonged recovery from exertional desaturation following a 6MWT was associated with worse baseline lung function and a higher risk of disease progression in patients with fILD.
Led by Albina Tyker, M.D., of the Division of Respirology in the Department of Medicine at McMaster University, the study used data from 194 adults with fILD who completed a 6MWT at interstitial lung disease clinics at the University of Calgary and the University of Chicago. Of the cohort, 94 were from Calgary and 100 from Chicago, with median follow-up times of 20 months and 30.1 months, respectively.
The researchers looked to determine whether recovery time from exertional oxygen desaturation was associated with disease severity and future outcomes. They developed a recovery index that integrates three factors: the degree of oxygen desaturation during the 6MWT, the time required to recover to within 3% of baseline oxygen saturation, and the use of supplemental oxygen. Higher values reflect more prolonged recovery.
Exertional desaturation was defined as a drop of more than 3% from baseline oxygen saturation at the end of the walk test. Baseline lung function was assessed using pulmonary function testing performed within three months of the 6MWT and disease severity was characterized using established measures, including percent predicted forced vital capacity (FVC) and the interstitial lung disease–gender, age, physiology (ILD-GAP) score.
According to Tyker, the findings point to a novel recovery index (RI) as a potential prognostic tool that could complement existing risk stratification models.
“Across the combined cohort, a higher RI was consistently associated with lower baseline lung function and higher ILD-GAP scores, indicating more advanced disease,” the authors wrote.
The median RI differed between centers, measuring 2.62 among Calgary patients and 3.61 among those in Chicago. Among patients who experienced exertional desaturation, median RI values were substantially higher, at 7.69 and 7.35, respectively.
“The primary outcome was a composite measure of disease progression, defined as death, lung transplantation, or a decline of 10% or more in absolute forced vital capacity within 12 months,” the authors noted. “Secondary outcomes included lung transplant–free survival.”
In unadjusted analyses, an RI greater than 3.97 was associated with a significantly increased risk of the composite outcome in the combined cohort and particularly in the Chicago cohort. In Chicago patients, elevated RI was linked to more than a threefold higher risk of disease progression
A chief finding from the study showed that the association between RI and disease severity persisted after adjustment for confounding factors. For instance, higher RI values were significantly associated with lower percent predicted FVC at baseline and higher ILD-GAP scores in both cohorts.
Therefore, the findings suggest that prolonged recovery from exertional hypoxemia reflects underlying disease burden rather than transient physiologic variability, according to the study authors.
The researchers also explored whether incorporating RI into existing prognostic models could improve risk prediction. In doing so, when RI was combined with the ILD-GAP score, the ability to predict mortality and transplant-free survival modestly improved compared with ILD-GAP alone, although the incremental gain did not reach statistical significance.
The researchers emphasized the practical appeal of this kind of recovery index, noting that it could be applied to patients completing a 6MWT with or without supplemental oxygen and across fibrotic ILD subtypes.
“The RI represents a potential new prognostic tool, which can be used for patients completing 6MWT with or without supplemental [oxygen] and regardless of fILD subtype,” the authors wrote. “The measure is associated with disease severity and may be useful in predicting transplant-free survival and disease progression in clinical practice or research settings.”
The study’s authors acknowledged several limitations, including differences in cohort characteristics between the Calgary and Chicago populations and the lack of external validation. Therefore, they noted, independent studies will be necessary to confirm the clinical utility of RI and to define how best to integrate it into routine care.
Even so, the findings add an important new dimension to the interpretation of the six-minute walk test in fibrotic interstitial lung disease.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.