Weighing Ablation Options in Persistent, Large Atrium AF
Researchers compared radiofrequency ablation, cryoballoon ablation and the thoracoscopic maze procedure. After adjustments for age and left atrium diameter, they found no prognostic differences among the treatment strategies for atrial fibrillation.
A small, retrospective study of three ablative procedures for atrial fibrillation (AF) has found that none provides a clear advantage over the other in treatment for patients with persistent AF and a large left atrium (LA). An oversized left atrium is a condition that can develop with persistent AF.
The three procedures studied were radiofrequency ablation (RFCA), cryoballoon ablation (CBA), and thoracoscopic maze (TM). The lead author on the study published in
However, investigators did find that early recurrence following RFCA and CBA was predictive for late recurrence.
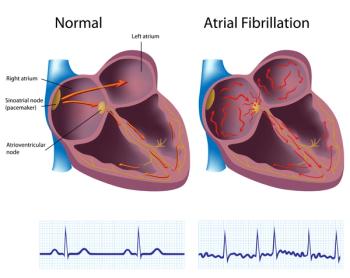
RFCA and CBA catheter procedures use heat and cold, respectively, to scar tissue and change the electrical conduction system of the heart. TM is a minimally invasive technique to scar the exterior of the heart to accomplish the same objective
Investigators said previous studies of this type have tended to focus on paroxysmal AF, short-term persistent AF (less than a year), and patients with a limited-size LA. “Therefore, it remains unclear which interventional strategy would be preferred for managing persistent AF patients with a large LA,” they wrote.
They screened records for patients with persistent AF with a large LA of a diameter greater than 50 mm. Patients fell into these treatment categories: RFCA, 32 (36.0%); CBA, 38 (42.7,%); TM, 19 (21.3%).
The average age was 63.5; about 80% were male; 17% had heart failure; 70%, hypertension; 21.3%, diabetes mellitus. On average, patients had received their diagnosis for AF 4.2 years prior to the ablation procedures.
Diabetes was more common in patients who underwent RFCA or CBA than in those who received TM.
Investigators said the differences in prevalence of heart failure and hypertension were not statistically significant across the groups.
During the three months following ablation, the TM group had higher early recurrence rates (89% vs 50% and 55.3% for RFCA and CBA, respectively).
Across all groups during the three-month period following ablation (blanking period), patients without late recurrence had lower left ventricular ejection fraction levels and lower early recurrence rates.
Investigators said that after adjusting for age and LA diameter, there were no prognostic differences across ablation strategies.
Also, no significant differences were found when stratifying patients for use of any antiarrhythmia drug medication.
At the 12-month follow-up, 48 incidents (53.9%) of persistent AF late recurrence were observed —o r more than half of all patients.
It is believed that early recurrence following ablation is caused by inflammation and therefore “is not a true AF recurrence.” However, investigators said this deserves a closer look. The risk of early recurrence was significantly higher in the TM group, and early recurrence was predictive of late recurrence in the RFCA and CBA groups.
“This suggests that the transient inflammatory status of LA after RFCA or CVA might be different from that of LA after thoracoscopic maze,” they concluded.
Limitations of the study include that it enrolled only East Asian patients and extrapolation to other ethnicities is needed. Also, it was a small retrospective cohort study and further, prospective studies are needed to validate the findings, the authors said.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.