Viral hepatitis C management involves some tough decisions
The best approach is to combine clinical therapy with strong support from behavioral health professionals.
From a care delivery standpoint, identifying and treating patients with the hepatitis C virus (HCV) is a complicated and difficult process. It's the most prevalent liver disease in the world, with as many as 300 million people afflicted with the virus worldwide, including as many as 5.8 million people in the United States alone.
Chronic HCV is a rapidly growing healthcare concern, considered by the World Health Organization to be an epidemic because 20% to 30% of people with the disease eventually will face life-threatening symptoms. It is the most common cause of chronic liver disease, accounting for 40% to 60% of all new cases. While hepatitis A and B also are significant healthcare issues, there are vaccines for both, making them bigger concerns in Third World and less-developed nations.
As many as 75% or more of patients with acute HCV ultimately will develop chronic infection, and most of those will deteriorate into chronic liver disease.
"There are people out there today who have no idea what is happening to their health, and many of them are people who 'cleaned up their act' decades ago," says Brian D. Klein, founder of the Hepatitis Action and Advocacy Coalition, a non-profit group based in San Francisco. "Unfortunately, the first information some of those people hear about it is when the doctor tells them they need a liver transplant."
"This disease has had, and will continue to have, a huge impact on healthcare, but we are hopeful that current and emerging treatments will help lower members' disease burden and result in lower rates of liver failure," says James Mackay, MD, medical director of Providence Health Plan, based in Beaverton, Ore. Its parent company, Providence Health System, provides healthcare services to more than 800,000 members throughout Oregon and Washington, and is the state's second-largest employer.
"Unfortunately," Dr. Mackay continues, "many patients do not respond to drugs, and many of those who respond initially have a relapse. Clearly, better therapies are needed."
While there are effective medical and pharmacological treatments already in existence and more surely on the way, the best approach is to combine clinical therapy with strong support from behavioral health professionals, because the impact of chronic HCV infection affects the mind almost as much as the body.
TREATMENT COSTS AND BENEFITS
The cost of treating HCV patients is expected to become a major burden on the healthcare system, as patients who are currently asymptomatic or have minor symptoms progress to end-stage liver disease and develop hepatocellular carcinoma.
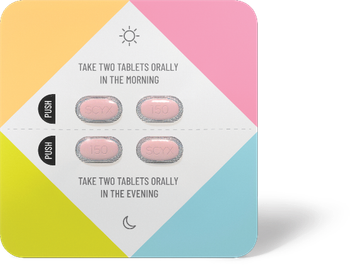
The currently accepted standard of care is combination therapy of pegylated interferon, an injectable drug, and ribavirin, an oral medication. Treatment results in sustained response rates of 40% to 80%. Industry estimates put the cost of therapy at $30,000 per year or more.
"We have a superb network of gastro-intestinal specialists who are quite knowledgeable about HCV and its therapy," Dr. Mackay says. "We rely upon them for management of the drugs and disease itself. Providence insists on specialty care for this disease because its effects and impact are so complex."
The cost of HCV treatment compares favorably to interventions routinely used for other diseases such as coronary bypass surgery, medications to combat high blood pressure, and mammography. The accepted measure of "effectiveness of treatment" is in life expectancy.
Generally, bypass surgery buys the patient about a year, while Pap smears and stool guaiac screenings add a few months. Eliminating coronary artery disease among 35-year-olds in the U.S population would increase life expectancy by about three years.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.