Intense family programs address motivation to reduce risk associated with weight
One case of a mother and child shows promise in family-oriented weight management and risk reduction
Clinical presentation usually centers around this group of conditions. Consider the following case study of a mother and child.
THE MOTHER
Her past medical history includes two pregnancies, both complicated by gestational diabetes. Both of her children had weights at birth that exceeded nine pounds. Her family history includes obesity in both parents and her children. Her father died of complications of diabetes.
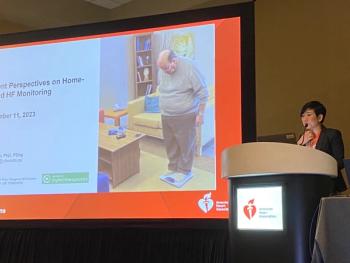
At her physical exam, she had an elevated blood pressure, was obese and had a Body Mass Index (BMI) well above a healthy range. Her waist circumference was 45 inches.
Laboratory studies showed elevated blood sugar, high cholesterol, triglycerides and a high hemoglobin A1c of 8.8%, (normal is 4% to 6%). She was placed on a weight-loss diet and exercise program for six weeks. On a return visit, her weight was unchanged. Her fasting blood sugar was elevated as well.
She was started on metformin, instructed on glucose monitoring and was scheduled for follow-up.
Through the next year, she continued to show elevated blood glucose levels and was not able to lose weight. She was started on a sulfonylurea, and warned that if her diabetes control worsened she would require insulin shots.
THE CHILD
C.V.'s son, J.V. (initials used to protect patient's privacy), was a seven-year-old boy who had been overweight for most of his life, and during the previous year had gained 32 pounds.
He had multiple hospital admissions for asthma. Over the previous year, he had spent several weeks in the pediatric ICU for status asthmaticus. He was on multiple medications for asthma; for the past year had been on three courses of prednisone.
His physical exam showed that he was tall for his age and had a high BMI, indicating obesity. His waist measured 36.2 inches. Vital signs showed high blood pressure. His physical exam showed a diminished lung capacity and wheezing, and darkening of the neck area and the underarm area, called acanthosis nigricans. He had liver enlargement.
Initial laboratory studies showed normal glucose levels, but abnormally high cholesterol and triglycerides. In addition his diabetes marker, Hgb A1c, was elevated, but not yet diabetic.
He also had elevated liver enzymes, indicating non-alcoholoic liver disease, seen in some obese children.
He and his family were referred to participate in a proprietary weight loss program. This program, approved by the state Medicaid program for the treatment of childhood obesity, was taught by a dietitian, a social worker and exercise instructor, lasting for eight weeks. The program is based on four principles:
The family attended three, eight-week sessions. During that time, the child lost 28 pounds. His lab studies showed a marked improvement, including a return to normal cholesterol and triglyceride levels, and his diabetes marker fell into the normal range. Additionally, his liver enzymes returned to normal, showing that his liver was restored.
His asthma abated, and during the time that he attended the weight-loss program, he was not hospitalized for asthma. His medical expenses related to asthma were significantly reduced.
In addition, his mother, C.V., noted in the first patient example, lost more than 20 pounds. Her blood pressure fell, and her attending physician took her off blood pressure medications. Also her dosage of diabetes medications was reduced. She was told that she may soon be able to stop her oral medications, and that she will not require insulin for management of diabetes.
METABOLIC DISORDERS
The epidemic of childhood obesity portends a flood of medical problems for this generation of children, even before they reach adulthood. The seeds of cardiovascular disease are already present in the obese seven-year-old patient's example, and appeared at a much younger age in him than they did in his mother. Some have speculated that this might be the first generation where children do not outlive their parents. The seriousness of this problem requires creative efforts of many to find a solution, if we are to save future generations from costly and deadly medical problems.
Childhood obesity is also associated with worsening childhood asthma, as illustrated in this case. The expenses related to the care of children with asthma drain healthcare dollars. The cost of treating childhood obesity, when associated with asthma would result in immediate and substantial savings of healthcare dollars.
Directing adults into weight loss programs is often difficult. They typically lack motivation, time and/or financial resources. The treatment of the adult with obesity has shown limited success. As seen in this case, the adult involved remained obese.
By linking the health of the child with the parent, the parent has a vested interest in improving the life and health of the child. As shown here, the interaction between the parent and child strengthens the motivation of the adult.
Managed care executives should consider:
Naomi D. Neufeld MD, FACE, is a pediatric endocrinologist and founder and CEO of the non-profit KidShape Foundation, Los Angeles.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.