Experts weigh in on the spending outlook for these high-cost conditions.
Mari Edlin is a frequent contributor to Managed Healthcare Executive. She is based in Sonoma, California.
Experts weigh in on the spending outlook for these high-cost conditions.

A lack of national standards and less than optimal oversight of many inpatient, opioid addiction rehabilitation programs is raising questions about the level of services, personnel, and quality of care many patients are receiving.

Find out what challenges top the list, and what analysts say can be done about them.

Prepare for major pipeline developments in diabetes, autoimmune disorders, oncology, and COPD.

PBMs partnering with pharmacies and drug makers may have a solution to nonadherence due to high pharma costs.

Polypharmacy presents real problems-especially for older adults.

Despite front-end scrutiny, payers seek audit process to improve high-cost specialty pharmacies.

Part D program exceeds industry expectations

Oncology pathways can lead to quality programs and more cost-effective care for cancer patients.

Generic drugs have certainly made their mark, but don't count on the same savings in the specialty market.

Retirees can expect to shoulder more than half of the cost burden of health benefits-51% to 54%-according to Towers Watson's 2010 Retiree Health Care Cost Survey.

Physician assistants (PAs) and nurse practitioners (NPs) could solve the shortage of primary care physicians and the rising cost of healthcare.

Dig into the minds of members and you'll find that they don't always make logical choices. Behavioral economics can shed light on their thought process

Only 20% of PDPs will offer gap coverage, and even then, most are limited to generics. House and Senate bills aim to help out.

Healthcare is funded by taxes and subsidies, but privately insured people are encouraged to buy upgrades

Physicians must evaluate the use of antidepressant medications based on new guidelines from two gynecological organizations

Recognize the interrelated health risks among four prevalent conditions to better manage big-picture treatment goals

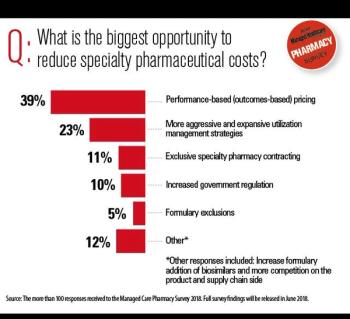
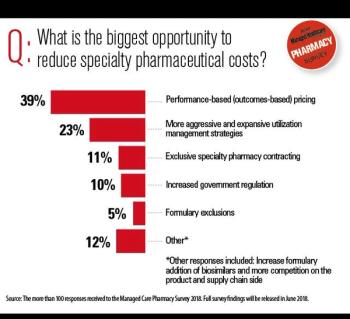
Outcomes-based contracting enables risk sharing between plans and manufacturers while also allowing better patient adherence to regimens

The healthcare industry has yet to use evidence-based medicine (EBM) to its fullest potential, despite studies suggesting the need for it. Wide variation in medical practice and resulting clinical outcomes is indicative of the not-yet completed journey toward implementing evidence-based medicine.

Biogenerics will not be taking the U.S. marketplace by storm any time soon. Approval of biogenerics is creating a rift between innovators and generic manufacturers and is putting data exclusivity and interchangeability to the test

What works for retail pharmacy patients should work for mail-order recipients, namely, personalized drug counseling. When consumers pick up their prescriptions at a local pharmacy, they have access to pharmacists who can advise them on how and when to take medications, warn them of potential side effects and discuss generic alternatives.

For payers struggling with unmanageable cost increases in the business of delivering care, however, price cannot be overlooked. Insurers don't necessarily deny coverage of a treatment just because it's expensive, but they would be remiss if they didn't take cost into consideration, as well as safety and effectiveness.

Groups such as WellPoint are turning specialty pharmacy into a highly beneficial business model for everyone from the non-clinician to physicians.

Some health insurers are hoping that new benefit designs targeting individuals will attract some of the uninsured and the self-employed, who either don't realize that they can get insurance or don't know how much they can afford.

As health plans elect to cover a new FDA-approved vaccine that protects girls and women against strains of the human papillomavirus (HPV), parents might wonder if it will be mandated by states as a routine immunization for girls at a certain age.

The centers for Medicare and Medicaid (CMS) says that 23% of Medicare beneficiaries have five or more chronic conditions but account for 68% of costs-not quite the 80/20 rule. And they tend to see many different doctors-about 14 a year with almost 40 office visits-and take as many as 10 medications at a time, according to Partnership for Solutions.

Disease management programs aimed at enhancing quality of life for older adults with multiple chronic illnesses are blossoming and are expected to experience future growth.

Last year acknowledged the 25th year since AIDS was first recognized, and to coincide with that anniversary, the U.S. Centers for Disease Control and Prevention (CDC) revised its recommendations for HIV testing for adults, adolescents and pregnant women in healthcare settings. The new guidelines remove the onus of determining who is at high risk for HIV infection and makes testing a routine part of medical care for all patients between ages 13 and 64 years.

CDC's revised HIV recommendations that all people aged 13 to 64 should have routine HIV testing may be effective in the public health setting, but might not be as effective in the privat setting, according to one expert.

Although as many as 48% of seniors were subject to some type of drug-coverage deficiency in 2006, only an estimated 4 million of the 22.5 million enrolled in Medicare drug plans were actually expected to hit the infamous donut hole. There could still be financial woes, however, for the 10.8 million Medicare beneficiaries who at least have the potential for out-of-pocket costs in the donut hole gap because they do not qualify for a subsidy, are not covered outside Part D, or did not pay for enhanced gap coverage.

Published: December 13th 2017 | Updated:

Published: April 8th 2017 | Updated:

Published: September 6th 2017 | Updated:

Published: September 1st 2004 | Updated:

Published: October 1st 2004 | Updated:

Published: October 1st 2004 | Updated: